 A case study examining the impact of non-combat casualties in the AIF during the First World War using data derived from service records of the 154 men of the 5th Reinforcements, 22nd Infantry Battalion, death records for the 22nd Battalion, and referenced against the published literature found in the ‘Official History of the Australian Medical Services, 1914-1918’. The findings will highlight the particular challenges faced in the different theatres of operation as the Great War progressed from its outbreak in 1914 to the Armistice of 1918.
A case study examining the impact of non-combat casualties in the AIF during the First World War using data derived from service records of the 154 men of the 5th Reinforcements, 22nd Infantry Battalion, death records for the 22nd Battalion, and referenced against the published literature found in the ‘Official History of the Australian Medical Services, 1914-1918’. The findings will highlight the particular challenges faced in the different theatres of operation as the Great War progressed from its outbreak in 1914 to the Armistice of 1918.
Historical context
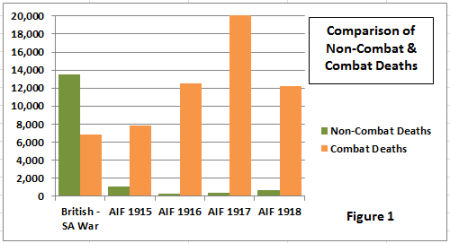 Discussion of war casualties tends to focus on the numbers killed or wounded in combat, however history is filled with campaigns where losses caused by non-combat related issues of disease and illness had a greater impact on the outcome. A century before the Great War, Napoleon Bonaparte marched his French Army of 600,000 men into Russia, but by the time they had retreated back into Poland this once proud army had been reduced to just 100,000, the majority having succumbed to exhaustion and exposure due to the lack of food and the harsh conditions of the Russian winter. From the mid-1800’s when the British began to keep detailed military medical records, every military campaign of that century had more hospital admissions for non-combat than combat causes, plus a soldier was more likely to die from illness or disease than on the battlefield. This included Crimea in the 1850’s and the Boer War in South Africa – as shown above in comparison of non-combat and combat deaths (Figure 1 – click on the figures to expand) and hospitalisation (see Figure 2 below) – just a decade before the start of the First World War, and in which a number of the original AIF were veterans.
Discussion of war casualties tends to focus on the numbers killed or wounded in combat, however history is filled with campaigns where losses caused by non-combat related issues of disease and illness had a greater impact on the outcome. A century before the Great War, Napoleon Bonaparte marched his French Army of 600,000 men into Russia, but by the time they had retreated back into Poland this once proud army had been reduced to just 100,000, the majority having succumbed to exhaustion and exposure due to the lack of food and the harsh conditions of the Russian winter. From the mid-1800’s when the British began to keep detailed military medical records, every military campaign of that century had more hospital admissions for non-combat than combat causes, plus a soldier was more likely to die from illness or disease than on the battlefield. This included Crimea in the 1850’s and the Boer War in South Africa – as shown above in comparison of non-combat and combat deaths (Figure 1 – click on the figures to expand) and hospitalisation (see Figure 2 below) – just a decade before the start of the First World War, and in which a number of the original AIF were veterans.
 The health of the armed forces with respect to what was dispassionately called ‘wastage’ was thus becoming an important issue for military strategists. Following her experience in Crimea nurse Florence Nightingale (photograph left) later wrote to the Secretary for India, Lord Salisbury, about the promotion of health in the British Army, quoting the Crown Prince Frederick of Germany as having said “We could add to the strength and numbers of organised armies by sanitary works. Money spent on these works contributed to military forces as much as fortifications and direct military organisation.”
The health of the armed forces with respect to what was dispassionately called ‘wastage’ was thus becoming an important issue for military strategists. Following her experience in Crimea nurse Florence Nightingale (photograph left) later wrote to the Secretary for India, Lord Salisbury, about the promotion of health in the British Army, quoting the Crown Prince Frederick of Germany as having said “We could add to the strength and numbers of organised armies by sanitary works. Money spent on these works contributed to military forces as much as fortifications and direct military organisation.”
Since the British – South African and Russo – Japanese Wars of the early 20th Century there had been some twelve years of medical observation and research, through which additional knowledge had been gained concerning the nature of various diseases. Underpinning this was the need to promote the general health and well-being of the soldier through a balanced and suitable diet, clothing, rest, warmth, and other factors in the promotion of physical well-being and morale. In addition the First World War coincided with the early stages of advancement in the science and art of medicine, both in terms of prevention, surgery and treatment that would lead to a dramatic fall in fatalities compared with earlier conflicts as can be seen in Figure 1. As a result the armies of Europe, although facing an industrialised war of destruction on a scale never before seen, embarked on the Great War at an advantage at least in respect to the control of disease.
Although the scourges of campaigns of the previous century such as smallpox, typhoid and cholera had been addressed and pretty much eliminated through vaccination and sound water management, the environment in which soldiers had to live was conducive to the outbreak of numerous other transmittable diseases. The fatality risk was a lot lower with these diseases however they did have a large impact on wastage and hence fighting 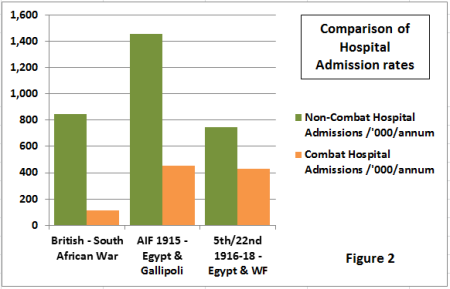 capability of each unit as can be seen in the hospital admissions shown in Figure 2 (represented per 1,000 men per annum for comparison). Here it can be seen that the hospital admissions per 1,000 men were higher for the AIF in Gallipoli than for the British in South Africa. A comparable figure for the AIF on the Western Front is not available, but the case study group of the 5th/22nd on the Western Front shows a non-combat hospitalisation rate similar to that of South Africa. When these rates are multiplied by the full fighting force of the Armies of the First World War then it can be seen that the medical services were having to receive and treat millions of cases and the military strategists to ensure sufficient replacements.
capability of each unit as can be seen in the hospital admissions shown in Figure 2 (represented per 1,000 men per annum for comparison). Here it can be seen that the hospital admissions per 1,000 men were higher for the AIF in Gallipoli than for the British in South Africa. A comparable figure for the AIF on the Western Front is not available, but the case study group of the 5th/22nd on the Western Front shows a non-combat hospitalisation rate similar to that of South Africa. When these rates are multiplied by the full fighting force of the Armies of the First World War then it can be seen that the medical services were having to receive and treat millions of cases and the military strategists to ensure sufficient replacements.
Challenges within the AIF theatres of operation
The challenges faced by the Australian Army Medical Services and those of the other Armies fluctuated and evolved as the Great War took its course. In this section an outline of the conditions and changing challenges faced by the AIF can be seen from its formation in Australia in 1914, to the camps of Egypt, the disastrous Gallipoli campaign of 1915, followed by the move to the Western Front theatre of operations and the supporting camps and depots of southern England to the Armistice in 1918 and subsequent demobilisation.
Australia – recruitment and training camps
 Following the outbreak of war in August 1914, men primarily drawn from the militia and with previous military experience began to assemble at training grounds across Australia. The first Anzac contingent of 20,000 in the AIF 1st Division and Light Horse sailed within two months and up to this point and throughout the southern hemisphere summer of 1914-15 the conditions in the Australian training camps plus the medical personnel to deal with sicknesses were adequate. However by mid-1915 the rush of men enlisting after the Anzac Landing at Gallipoli reached a peak in July, when they totalled over 36,000 across the country, of which 21,698 were in Victoria. By October there were close to 74,000 troops in the overcrowded camps. At Broadmeadows Camp north of Melbourne the continuous rains converted the surface into mud, and with overcrowding in the unfloored tents, together with a lack of mess and drying huts, respiratory infections became prevalent. The troops were transferred to Seymour pending the reconstruction of the Broadmeadows Camp, but Seymour Camp itself became greatly overcrowded, and, in spite of improved hospital accommodation, deaths from pneumonia (directly or associated with influenza or measles) became frequent. Of the cases of disease reported among the troops in Australia from July 1915 to June 1916, 61 per cent were from respiratory and nasal infections, of which 20 per cent were measles, and 55 per cent influenza. Up to 30th June 1916, 604 cases of cerebro-spinal meningitis had occurred among the recruits (an incidence at least five times greater than that amongst the civil population) with 256 deaths – a mortality of 42.4 per cent. In total 693 deaths had occurred among recruits in training camps from the following causes: cerebro-spinal fever 256; pneumonia 191; accidents and injuries 74; pneumonia & broncho-pneumonia 29; tuberculosis 16.
Following the outbreak of war in August 1914, men primarily drawn from the militia and with previous military experience began to assemble at training grounds across Australia. The first Anzac contingent of 20,000 in the AIF 1st Division and Light Horse sailed within two months and up to this point and throughout the southern hemisphere summer of 1914-15 the conditions in the Australian training camps plus the medical personnel to deal with sicknesses were adequate. However by mid-1915 the rush of men enlisting after the Anzac Landing at Gallipoli reached a peak in July, when they totalled over 36,000 across the country, of which 21,698 were in Victoria. By October there were close to 74,000 troops in the overcrowded camps. At Broadmeadows Camp north of Melbourne the continuous rains converted the surface into mud, and with overcrowding in the unfloored tents, together with a lack of mess and drying huts, respiratory infections became prevalent. The troops were transferred to Seymour pending the reconstruction of the Broadmeadows Camp, but Seymour Camp itself became greatly overcrowded, and, in spite of improved hospital accommodation, deaths from pneumonia (directly or associated with influenza or measles) became frequent. Of the cases of disease reported among the troops in Australia from July 1915 to June 1916, 61 per cent were from respiratory and nasal infections, of which 20 per cent were measles, and 55 per cent influenza. Up to 30th June 1916, 604 cases of cerebro-spinal meningitis had occurred among the recruits (an incidence at least five times greater than that amongst the civil population) with 256 deaths – a mortality of 42.4 per cent. In total 693 deaths had occurred among recruits in training camps from the following causes: cerebro-spinal fever 256; pneumonia 191; accidents and injuries 74; pneumonia & broncho-pneumonia 29; tuberculosis 16.
 With this poor state of health within the camps steps were taken to improve the situation. Opportunity for infection from outside was limited by the abolition of night leave and of transfers from infected camps. A system of decentralisation was initiated, limiting the size of camps to 5,000 and in September 1915 a conference of specialists, presided over by the Commonwealth Director of Quarantine (Dr. J. H Cumpston) recommended as ‘essential’ the stamping out of the disease by the lessening of overcrowding.
With this poor state of health within the camps steps were taken to improve the situation. Opportunity for infection from outside was limited by the abolition of night leave and of transfers from infected camps. A system of decentralisation was initiated, limiting the size of camps to 5,000 and in September 1915 a conference of specialists, presided over by the Commonwealth Director of Quarantine (Dr. J. H Cumpston) recommended as ‘essential’ the stamping out of the disease by the lessening of overcrowding.
However the camp environment was still providing a fertile breeding ground for contagious diseases such as mumps and measles and were, unbeknown at the time, creating a later problem for the AIF Depots in Egypt and the UK. In 1917 a policy was introduced whereby all drafts from Australia were placed for 14 days in an isolation zone to continue their training before embarking for overseas. If a case later broke out on the transport then they were put in isolation, and as a result the numbers of cases dropped dramatically. In 1917 the average number of cases of mumps in hospital decreased from 800 to 200, and in the first half of 1918 to 62. The great success of this policy was shown that from June 1917 to December 1918 not a single case of mumps and only five cases of measles got to France among nearly 100,000 reinforcements.
Within the 22nd Battalion two men died while at sea on route from Australia to Egypt with the first contingent in May 1915 – Pte Matheson of kidney failure and Pte Lauder of heat exhaustion. Through the war one member of the 22nd Battalion would die of illness in Australia in each of the four remaining years – Pte Colvin, meningitis (1916); Pte Westwood, tuberculosis (1917); Pte Warrener, tuberculosis (1918); Lieut. Wymond, influenza (1919). In addition five former members of the 22nd Battalion died after discharge in 1920 from conditions unknown.
Egypt – training camps and base for Gallipoli
Between the arrival of the General Bridges and first AIF contingent at the end of 1914 to the departure of the four infantry divisions to France in March 1916, Egypt acted as the base and training depot for the Australian Imperial Force in supporting their operations in Gallipoli in 1915 and preparing for the transfer to Europe and the Western Front. For the medical services, Egypt was the primary location for the wounded and sick from Gallipoli, with the most serious cases remaining in Alexandria in the British general hospitals, which many regarded as the best in the British Army. The less injured plus in the early days the greater proportion of the sick were sent to Cairo, but with over 22,000 sick and wounded arriving in August alone, the medical services were soon stretched to breaking point. The situation was alleviated by the arrival of Atlantic liners that would take many of the casualties to Malta and further to England, plus the establishing of the 3rd Australian General Hospital and two Stationary Hospitals on the Greek island of Lemnos.
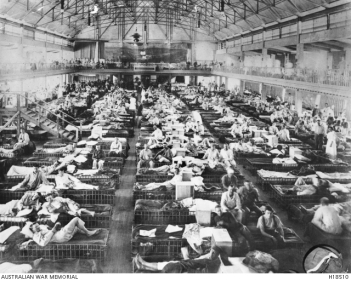 However as well as receiving both the combat and non-combat casualties from Gallipoli the medical services also had to deal with sickness outbreaks occurring within the camps in Egypt. Right from their arrival in late 1914 there had been a sudden outbreak of respiratory infections in the camps, the causes of which were brought by the AIF 1st Division from Australia, but it was during the last four months of 1915 that the Australian medical units in Egypt became more and more occupied in the treatment of local sick, the two general hospitals (1AGH and 2AGH) and their Auxiliaries acting as camp hospitals to an increasing number of Australian troops in Egypt.
However as well as receiving both the combat and non-combat casualties from Gallipoli the medical services also had to deal with sickness outbreaks occurring within the camps in Egypt. Right from their arrival in late 1914 there had been a sudden outbreak of respiratory infections in the camps, the causes of which were brought by the AIF 1st Division from Australia, but it was during the last four months of 1915 that the Australian medical units in Egypt became more and more occupied in the treatment of local sick, the two general hospitals (1AGH and 2AGH) and their Auxiliaries acting as camp hospitals to an increasing number of Australian troops in Egypt.
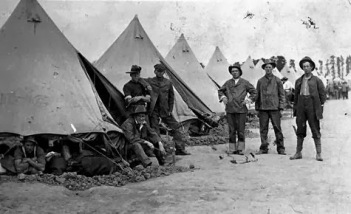
With the exception of Alexandria, where the Medical Advisory Committee found that a large proportion of the enteric and dysenteric infection was derived from the Dardanelles, at the camps the causes of gastro-intestinal and jaundice cases were derived from the same local sources endemic in Egypt. On the initiative of an Australian medical officer the use of heavy petroleum oils in effective quantity was used at Zeitoun Camp for covering waste, but it took to the end of 1915 before anti-fly measures were taken on a systematic basis. The outbreaks of respiratory infections on the other hand coincided with the arrival  of the transports and reinforcements from Australia. The Australian medical services recognised that the chief source of respiratory outbreaks was the inadequate provision made in Australia to identify and quarantine incubating cases and infections amongst the embarking troops. When in Egypt the close proximity of the soldiers in the tents and the fluctuating extremes in daily temperatures led to an environment where respiratory disease could easily be developed. As a consequence, respiratory infections became so rampant that in October No. 4 Auxiliary Hospital was opened for this type of infection and by the end of the 1915 had taken 2,331 cases, including 1,439 mumps and 228 measles. One such casualty of the mumps was Capt. Evans (photograph left), the popular senior officer when the 5th/22nd departed for Egypt. The timing of his sickness meant that he was hospitalised during the period that the 22nd Battalion was conducting its final preparations for France and as a result he was transferred to the 8th Battalion that sailed later in March 1916. Capt Evans was later awarded the Military Cross before being killed in action at Polygon Wood during the 3rd Ypres campaign.
of the transports and reinforcements from Australia. The Australian medical services recognised that the chief source of respiratory outbreaks was the inadequate provision made in Australia to identify and quarantine incubating cases and infections amongst the embarking troops. When in Egypt the close proximity of the soldiers in the tents and the fluctuating extremes in daily temperatures led to an environment where respiratory disease could easily be developed. As a consequence, respiratory infections became so rampant that in October No. 4 Auxiliary Hospital was opened for this type of infection and by the end of the 1915 had taken 2,331 cases, including 1,439 mumps and 228 measles. One such casualty of the mumps was Capt. Evans (photograph left), the popular senior officer when the 5th/22nd departed for Egypt. The timing of his sickness meant that he was hospitalised during the period that the 22nd Battalion was conducting its final preparations for France and as a result he was transferred to the 8th Battalion that sailed later in March 1916. Capt Evans was later awarded the Military Cross before being killed in action at Polygon Wood during the 3rd Ypres campaign.
Towards the end of the year pneumonia also became prevalent but never assumed the epidemic features of the preceding winter when 41 of the 69 deaths were from this disease. After gastro-intestinal and respiratory infections venereal disease constituted the next highest cause of hospitalisation in Egypt, not helped by the initial liberal and goodwill attitude of High Command for the Australians to venture into Cairo on leave and to spend their money in the local economy. With the departure of 1st Division to Gallipoli, the Australians moved their base camp from Mena near Cairo to the middle of the desert and closer to the Suez Canal, thereby reducing opportunities of temptation in the city.
 For the 5th/22nd there were a total of 44 cases of hospital admissions from their arrival from Australia in October 1915 to their departure for France in mid-March 1916. These admissions were for a variety of conditions prevalent in the camps including mumps, measles, influenza, diarrhoea, gastro-enteritis and venereal disease. Included amongst the non-combat casualties were 2394 Pte Stephens (photograph left, standing) who was admitted to hospital soon after arriving in Egypt with diarrhoea, and 2397 Pte Samways (seated) who was admitted twice, with enteritis in November and then dysentery in December. Both Pte Stephens (later wounded four times and awarded the Military Medal) and Pte Samways (wounded once at Pozieres) survived the war.
For the 5th/22nd there were a total of 44 cases of hospital admissions from their arrival from Australia in October 1915 to their departure for France in mid-March 1916. These admissions were for a variety of conditions prevalent in the camps including mumps, measles, influenza, diarrhoea, gastro-enteritis and venereal disease. Included amongst the non-combat casualties were 2394 Pte Stephens (photograph left, standing) who was admitted to hospital soon after arriving in Egypt with diarrhoea, and 2397 Pte Samways (seated) who was admitted twice, with enteritis in November and then dysentery in December. Both Pte Stephens (later wounded four times and awarded the Military Medal) and Pte Samways (wounded once at Pozieres) survived the war.
Prior to their departure for Gallipoli in September 1915, the 22nd Battalion had five men die from disease while in Egypt – Pte Sommerville, Pte Dean and Pte Cobham from diphtheria, Pte Bunting from septicaemia and Pte Barton from broncho-pneumonia. Between January 1915 and March 1916 a total of 11,509 men within the AIF embarked from Alexandria in Egypt for return to Australia. Of these just 208 were combat casualties from Gallipoli. The rest were 6,365 sick, 1,352 with venereal diseases, and 1,584 others, including three members of the 5th/22nd deemed unfit for further service overseas.
Gallipoli – campaign of 1915
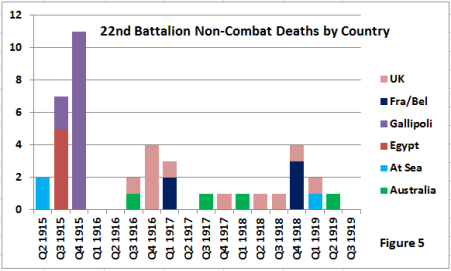
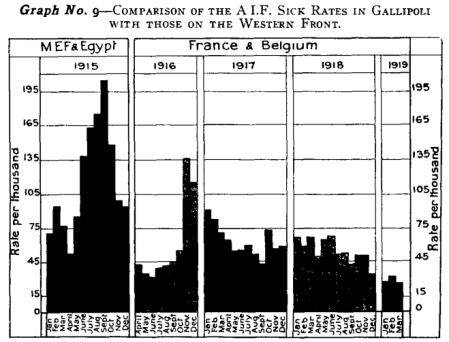 Gallipoli was the most trying time for the men of the AIF from disease and illness within the First World War. This period saw the highest rate of non-combat hospital admissions per months in the war (see ‘Graph 9’: Comparison of sick rates between Gallipoli and the Western Front – source ‘Official History of the Australian Medical Services, 1914-1918’), with a total of 1,455 cases per thousand troops. In addition the diseases were the most serious if not treated promptly, leading in 1915 to the highest number of non-combat deaths for the AIF with a total of 1,121 compared with 1,402 in total for the following three years on the Western Front, as shown previously in Figures 1 & 2 above. This high non-combat death figure can also be illustrated in Figure 5 below where in the three months on the front line leading up to the December evacuation, a total of thirteen men from the 22nd Battalion died from sickness contracted at Gallipoli, more than for the whole of 1917 and 1918 combined.
Gallipoli was the most trying time for the men of the AIF from disease and illness within the First World War. This period saw the highest rate of non-combat hospital admissions per months in the war (see ‘Graph 9’: Comparison of sick rates between Gallipoli and the Western Front – source ‘Official History of the Australian Medical Services, 1914-1918’), with a total of 1,455 cases per thousand troops. In addition the diseases were the most serious if not treated promptly, leading in 1915 to the highest number of non-combat deaths for the AIF with a total of 1,121 compared with 1,402 in total for the following three years on the Western Front, as shown previously in Figures 1 & 2 above. This high non-combat death figure can also be illustrated in Figure 5 below where in the three months on the front line leading up to the December evacuation, a total of thirteen men from the 22nd Battalion died from sickness contracted at Gallipoli, more than for the whole of 1917 and 1918 combined.
 Napoleon had understood that “an army marches on its stomach” but could do little to influence the outcome. At Gallipoli the supply and distribution of food, fuel and water for the maintenance of its men, animals, and machines was a problem of the most extreme complexity in this campaign due to its remote location and the need to supply the Peninsula by sea. The problem for the Australians and the Allies in general at Gallipoli were compounded by the narrow toehold that they had on this harsh, barren land restricting their ability to provide the necessary logistical support including safe medical facilities, sanitation, rest and cooking facilities, and waste disposal.
Napoleon had understood that “an army marches on its stomach” but could do little to influence the outcome. At Gallipoli the supply and distribution of food, fuel and water for the maintenance of its men, animals, and machines was a problem of the most extreme complexity in this campaign due to its remote location and the need to supply the Peninsula by sea. The problem for the Australians and the Allies in general at Gallipoli were compounded by the narrow toehold that they had on this harsh, barren land restricting their ability to provide the necessary logistical support including safe medical facilities, sanitation, rest and cooking facilities, and waste disposal.
After the early August 1915 attacks at Lone Pine and The Nek, the history of the Dardanelles campaign is almost entirely concerned with disease and its effects. The rush of wounded from the summer offensive was followed in late-August, September, and October, by a flood of sick which far surpassed all expectations and brought about an acute cry for reinforcements at the front and a renewed crisis on the lines of communication and at the bases. In August the AIF 1st Division suffered a loss of 57% of its force of which 32% were sick, and when the Assistant Director Medical Services called for special report from his regimental medical officers their unanimous response was one of gravest concern – “Men were just skin and bone, with hands, arms, and legs covered with septic sores and ill with dysentery. I have never seen men out of hospital looking so ill as a large proportion of the men here do. Men frequently faint at their posts.”
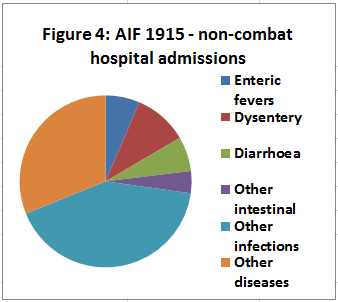 The ill health of the troops at this time was mainly diarrhoea, mild dysentery, influenza, debility as a result of the prolonged occupation of trenches under fire, and also by war diet of bully-beef, bacon, and biscuits to which men were unaccustomed. The collapse in health of the AIF 1st Division troops, after extended service in this inhospitable terrain, at last compelled their relief by fresher units. However the predominately fly-borne causes of disease brought about by the poor sanitation on the peninsula – water was the initial suspicion and thus the focus of attention when the first wave of cases occurred in June and July – had gone too long undiscovered and unchecked, hence the newly-arrived troops in the AIF 2nd Division went sick even more quickly than the older ones. During the hot summer months the air was thick with flies, making it practically impossible to eat without the contaminated pests landing on and infecting the food, and as the men filed to the latrines the source for contamination increased. In addition the desire to retain slight cases at the front for military reasons increased the spread of infection, and when the nature and cause were realised the outbreak was beyond control. Research into the causes did result in the use of Emetine to treat cases, but it would not be the woefully inadequate precautions but the onset of winter and the dying off of the flies that would put an end to the wave of intestinal disease.
The ill health of the troops at this time was mainly diarrhoea, mild dysentery, influenza, debility as a result of the prolonged occupation of trenches under fire, and also by war diet of bully-beef, bacon, and biscuits to which men were unaccustomed. The collapse in health of the AIF 1st Division troops, after extended service in this inhospitable terrain, at last compelled their relief by fresher units. However the predominately fly-borne causes of disease brought about by the poor sanitation on the peninsula – water was the initial suspicion and thus the focus of attention when the first wave of cases occurred in June and July – had gone too long undiscovered and unchecked, hence the newly-arrived troops in the AIF 2nd Division went sick even more quickly than the older ones. During the hot summer months the air was thick with flies, making it practically impossible to eat without the contaminated pests landing on and infecting the food, and as the men filed to the latrines the source for contamination increased. In addition the desire to retain slight cases at the front for military reasons increased the spread of infection, and when the nature and cause were realised the outbreak was beyond control. Research into the causes did result in the use of Emetine to treat cases, but it would not be the woefully inadequate precautions but the onset of winter and the dying off of the flies that would put an end to the wave of intestinal disease.
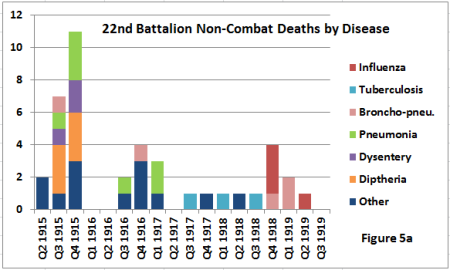 By October the picture was changing with fewer dysentery cases but with jaundice, respiratory and diphtheria cases increasing, reflecting outbreaks in Egypt and originating from epidemics in Australia. Tented ‘infectious’ hospitals were created at Anzac but were overcrowded and not immune to the danger from shelling. From September onwards anti-tetanus injections were given for every variety of wound. For the 22nd Battalion in the three months on the front line leading up to the December evacuation, a total of thirteen men died from sickness contracted at Gallipoli with, as can be seen in Figure 5a above, the most common causes being pneumonia, diphtheria and dysentery.
By October the picture was changing with fewer dysentery cases but with jaundice, respiratory and diphtheria cases increasing, reflecting outbreaks in Egypt and originating from epidemics in Australia. Tented ‘infectious’ hospitals were created at Anzac but were overcrowded and not immune to the danger from shelling. From September onwards anti-tetanus injections were given for every variety of wound. For the 22nd Battalion in the three months on the front line leading up to the December evacuation, a total of thirteen men died from sickness contracted at Gallipoli with, as can be seen in Figure 5a above, the most common causes being pneumonia, diphtheria and dysentery.
Western Front – i) Classification of diseases
To help in the prevention and treatment of the diseases and ailments faced during the First World War, by the time the AIF moved to the Western Front in March 1916 the Australian Army Medical Services used a classification system to group the diseases. There were eight types which were then sub-divided into classes, the most common of which are shown in Table 1 below:
Table 1: Disease Classification for the AIF, Western Front, 1916-1918
| Type | Description | Main Classes | Admissions | % |
| I | Defects & deformities of civilised life | Age factors; structural defects; dental defects | 7,349 | 3.47 |
| II | Accidental injuries on service | All accidental injuries | 15,648 | 7.39 |
| III | Primary infections and infestations by living agents | Respiratory tract infections; skin infestations; PUO; septic infections; venereal disease | 121,151 | 57.19 |
| IV | Psycho-physical factors – environment, nutrition & fatigue | Heat & cold; physiological hardships; psycho-physical exhaustion | 36,636 | 17.30 |
| V | Disorders of the mind | Psychic environment | 7,205 | 3.40 |
| VI | Metabolic diseases, disorders | Allergies | 1,217 | 0.58 |
| VII | Secondary dysfunctions and degenerations and terminal states | Impaired constitution; digestive system; organs of special sense; skin | 21,007 | 9.91 |
| VIII | Sundries, undiagnosed, and unintelligible | 1,609 | 0.76 |
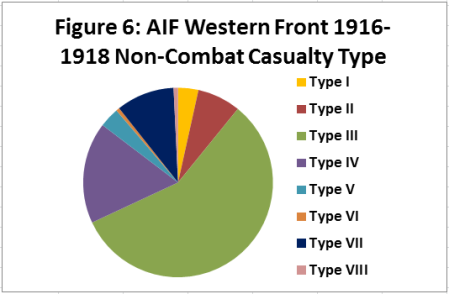 The data collected from admissions to the Field Ambulances in France and Belgium between April 1916 and March 1919 for the AIF on the Western Front as shown in Figure 6 illustrates that Types III, IV and VII made up about 85% of the total non-combat casualties. Of these Type III was responsible for over half of the cases and accounted for four out of the five sub-groups or classes. Breaking down further into the classes, the main causes for non-battle casualties for the AIF on the Western Front were as shown in Figure 7: respiratory tract infections with 41,300 cases (19.49%), of which influenza represented 21,947 cases (10.36%); PUO (Pyrexia of Uncertain Origin) with 24,593 cases (11.61%); Environment and fatigue with 24,223 (11.43%) of which trench foot was 7,202 (3.4%), and acute diarrhoea 7,121 (3.36%); Skin infestations 20,533 (9.69%) of which scabies was 19,920 cases (9.4%); and Venereal infections 13,105 (6.19%). The data from the 5th/22nd Battalion
The data collected from admissions to the Field Ambulances in France and Belgium between April 1916 and March 1919 for the AIF on the Western Front as shown in Figure 6 illustrates that Types III, IV and VII made up about 85% of the total non-combat casualties. Of these Type III was responsible for over half of the cases and accounted for four out of the five sub-groups or classes. Breaking down further into the classes, the main causes for non-battle casualties for the AIF on the Western Front were as shown in Figure 7: respiratory tract infections with 41,300 cases (19.49%), of which influenza represented 21,947 cases (10.36%); PUO (Pyrexia of Uncertain Origin) with 24,593 cases (11.61%); Environment and fatigue with 24,223 (11.43%) of which trench foot was 7,202 (3.4%), and acute diarrhoea 7,121 (3.36%); Skin infestations 20,533 (9.69%) of which scabies was 19,920 cases (9.4%); and Venereal infections 13,105 (6.19%). The data from the 5th/22nd Battalion 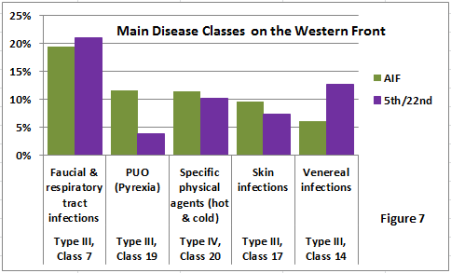 case study group are provided for comparison and show similar value with respect to respiratory tract infections, environment and fatigue, and skin infections. There are differences in frequency of admissions for PUO and also venereal disease. With regard to the latter, a previous case study paper on discipline within the AIF showed that the 5th/22nd had a worse discipline rate than the average for the AIF, and a number of the persistent illegal absentees (Absent Without Leave) that ended in Courts Martial and penal servitude were also repeat offenders for venereal disease, so a possible correlation between infection frequency and poor discipline.
case study group are provided for comparison and show similar value with respect to respiratory tract infections, environment and fatigue, and skin infections. There are differences in frequency of admissions for PUO and also venereal disease. With regard to the latter, a previous case study paper on discipline within the AIF showed that the 5th/22nd had a worse discipline rate than the average for the AIF, and a number of the persistent illegal absentees (Absent Without Leave) that ended in Courts Martial and penal servitude were also repeat offenders for venereal disease, so a possible correlation between infection frequency and poor discipline.
Western Front – ii) trench warfare in France & Belgium
Between March and June 1916 the Australian troops began arriving in France from Egypt with many having served in Gallipoli. In both prior locations the rate of sickness had been high and from highly contagious diseases not prevalent in Western Europe. To prevent the introduction of these diseases into France the following steps were taken: close sanitary  supervision in Egypt during a period of 3-4 months following the Gallipoli evacuation; before embarkation a vigorous campaign to free the force from lice with complete inspections; inoculation with T.A.B. (Typhoid) and re-vaccination against smallpox. In addition No.2 Australian General Hospital was established at Moussot, Marseille, and was well equipped for the isolation of any infectious disease identified through inspection prior to the disembarkation of the troops by the medical officer in charge of transports. This included 2426 Pte Turner of the 5th/22nd – (photograph left, from Lieut. Harricks collection) later to become Lieut. ‘mascot’ Turner and going through the rest of the war unscathed – who was admitted to hospital upon embarkation with tonsillitis. These measures proved to be successful with known leakage cases through the ‘Marseille sieve’ just a few in number. This action by the Australian Army Medical Services helped to deliver the dramatic reduction in hospital admissions and deaths recorded between the eastern Mediterranean theatre and the Western Front, as was seen in the deaths and non-combat casualty admissions in Figures 1 & 2 above.
supervision in Egypt during a period of 3-4 months following the Gallipoli evacuation; before embarkation a vigorous campaign to free the force from lice with complete inspections; inoculation with T.A.B. (Typhoid) and re-vaccination against smallpox. In addition No.2 Australian General Hospital was established at Moussot, Marseille, and was well equipped for the isolation of any infectious disease identified through inspection prior to the disembarkation of the troops by the medical officer in charge of transports. This included 2426 Pte Turner of the 5th/22nd – (photograph left, from Lieut. Harricks collection) later to become Lieut. ‘mascot’ Turner and going through the rest of the war unscathed – who was admitted to hospital upon embarkation with tonsillitis. These measures proved to be successful with known leakage cases through the ‘Marseille sieve’ just a few in number. This action by the Australian Army Medical Services helped to deliver the dramatic reduction in hospital admissions and deaths recorded between the eastern Mediterranean theatre and the Western Front, as was seen in the deaths and non-combat casualty admissions in Figures 1 & 2 above.
Keen to avoid the problems that dysentery had on the men in Gallipoli, every case of suspected dysentery was now investigated, and if positive, evacuated. All cases of diarrhoea were treated as suspect and as a result the potential carriers were controlled. The use of ‘fly proof’ latrines for faecal disposal was made a matter of discipline, though in front lines the covering of waste was often impossible to do. Other factors contributed to a better health situation on the Western Front including a greater variety of food and more hygienic cooking facilities, plus better facilities for personal cleanliness, and regular reliefs from the front line to rest areas some 5 – 15 kms to the rear. The measures taken above plus the change in physical environment meant that the disease profile for the Western Front changed, and with the decline of the serious diseases so did the death rate from non-combat sickness. For the 22nd Battalion the fatalities improved from the worst quarter in the war with eleven non-combat deaths to two subsequent quarters of zero deaths as shown in Figure 5 above.
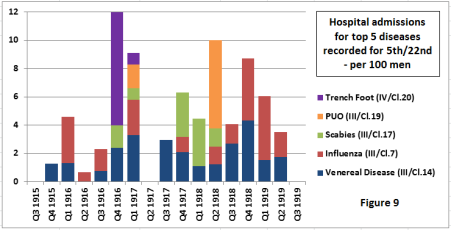
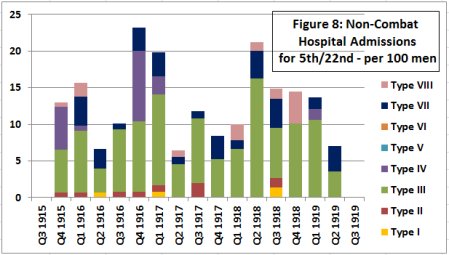 The Western Front posed challenges of a different nature to that faced previously. Five months of attritional fighting since 1st July 1916 had turned the Somme battlefield into a shell-cratered landscape that had wrecked the natural drainage of the land, so when the heavy rains of Autumn 1916 came the battlefield was turned into a quagmire of water and mud. With a lack of duck-boards and dry standing places the soldiers feet soon suffered from the wet and cold and developed what became known as ‘Trench Foot’ which if not treated quickly would turn toes and feet black leading to amputation. Within weeks troops were being evacuated from the forward area in large numbers. At the height in mid-November 1916 the forward AIF Divisions were evacuating around two hundred cases a week, or as seen in our case study group of the 5th/22nd eight cases per 100 men, the highest rate of any single sickness during the war and making the fourth quarter 1916 the highest in terms of non-combat wastage for the 5th/22nd (see Figure 8 ) and the AIF overall on the Western Front (see ‘Graph 9’ above). With the wastage situation becoming serious facilities for foot care were put in place, such as forward-placed drying areas, rubbing and increasing circulation, use of whale-oil, spare socks. The issue was raised to a level that the frequency of occurrence of this condition would reflect badly on the individual officers, their organisation and management, and the overall morale of the unit. These preventative measures helped but by the end of December mother nature had assisted in the reduction of this disease with the arrival of the winter frosts, and sickness and illness in this season reverted to those of cold, wet, malnutrition and exhaustion, i.e. the hardship of living in the forward area of a battlefield during winter.
The Western Front posed challenges of a different nature to that faced previously. Five months of attritional fighting since 1st July 1916 had turned the Somme battlefield into a shell-cratered landscape that had wrecked the natural drainage of the land, so when the heavy rains of Autumn 1916 came the battlefield was turned into a quagmire of water and mud. With a lack of duck-boards and dry standing places the soldiers feet soon suffered from the wet and cold and developed what became known as ‘Trench Foot’ which if not treated quickly would turn toes and feet black leading to amputation. Within weeks troops were being evacuated from the forward area in large numbers. At the height in mid-November 1916 the forward AIF Divisions were evacuating around two hundred cases a week, or as seen in our case study group of the 5th/22nd eight cases per 100 men, the highest rate of any single sickness during the war and making the fourth quarter 1916 the highest in terms of non-combat wastage for the 5th/22nd (see Figure 8 ) and the AIF overall on the Western Front (see ‘Graph 9’ above). With the wastage situation becoming serious facilities for foot care were put in place, such as forward-placed drying areas, rubbing and increasing circulation, use of whale-oil, spare socks. The issue was raised to a level that the frequency of occurrence of this condition would reflect badly on the individual officers, their organisation and management, and the overall morale of the unit. These preventative measures helped but by the end of December mother nature had assisted in the reduction of this disease with the arrival of the winter frosts, and sickness and illness in this season reverted to those of cold, wet, malnutrition and exhaustion, i.e. the hardship of living in the forward area of a battlefield during winter.
 Scabies, caused by the ‘itch mite’ was another significant cause of non-combat wastage on the Western Front with the main problem coming from infection of the affected part of the skin. Blankets and underwear were the two main vehicles of infection, and controlled by regular scabies parades, with treatment at the Field Ambulances, Casualty Clearing Stations as well as the Camiers General Hospital close to the AIF depot at Etaples. The incidences of scabies were reduced with the improvement of bathing facilities.
Scabies, caused by the ‘itch mite’ was another significant cause of non-combat wastage on the Western Front with the main problem coming from infection of the affected part of the skin. Blankets and underwear were the two main vehicles of infection, and controlled by regular scabies parades, with treatment at the Field Ambulances, Casualty Clearing Stations as well as the Camiers General Hospital close to the AIF depot at Etaples. The incidences of scabies were reduced with the improvement of bathing facilities.
At the end of 1916 the Director of Medical Services of the British Fourth Army required that along with trench foot and scabies, all cases of venereal disease be recorded. VD, a highly preventable disease, was particularly a problem for the Anzac Corps commanders with a higher rate of infection by Australian and New Zealand troops than any other nationality in the British Army. Despite education, the loss of pay, embarrassment should family members find out, and the prospect of rudimentary treatment this issue pervaded through the entire war, with infection most likely when on furlough or absconding from hospitals or camps while recuperating from wounds or sickness. During the first quarter of 1917, the average number in hospital from the AIF UK Depot was 7.5%, with almost half suffering from venereal disease. Repeat infection was deemed by some in authority as a deliberate attempt at self harming to avoid time at the front and for those men with a record of absenteeism, penal custodial sentences were issued to persistent offenders.
Another important cause of loss of manpower was Pyrexia of Uncertain Origin (PUO) or trench fever caused by the body louse. This disease, which affected large numbers of men but was not fatal, was largely preventable through careful inspection at frequent intervals, clean underwear, bathing and disinfestation. Extra attention was taken at the laundry stations to use the hot irons in all the creases and folds of soldier’s uniforms to kill the lice and their eggs.
 However in the Great War the weakness in preventative medicine, as it is today, was that of the susceptibility of the respiratory tract, with micro-organisms transported by droplets of mucus from coughing etc. Living in close overcrowded often damp conditions, with large changes in temperatures in the field, were perfect for the spread and development of diseases such as influenza and pneumonia. Of the total non-battle casualties admitted to field ambulance from the AIF on the Western Front, 19.5% (41,300 cases) were for respiratory diseases caused by parasitic infection or infestation. One such soldier that contracted influenza while in France was 2398 Sgt Strachan (photograph left) of the 5th/22nd. Sgt Strachan – the second highest decorated man in the 5th/22nd having been awarded the Distinguished Conduct Medal and Military Medal – also developed Trench Foot in November 1916 and German Measles while in camp in England waiting for his eventual return to Australia. Sgt Strachan was also wounded in action on the Somme in 1918 before eventually returning home to Australia in 1919.
However in the Great War the weakness in preventative medicine, as it is today, was that of the susceptibility of the respiratory tract, with micro-organisms transported by droplets of mucus from coughing etc. Living in close overcrowded often damp conditions, with large changes in temperatures in the field, were perfect for the spread and development of diseases such as influenza and pneumonia. Of the total non-battle casualties admitted to field ambulance from the AIF on the Western Front, 19.5% (41,300 cases) were for respiratory diseases caused by parasitic infection or infestation. One such soldier that contracted influenza while in France was 2398 Sgt Strachan (photograph left) of the 5th/22nd. Sgt Strachan – the second highest decorated man in the 5th/22nd having been awarded the Distinguished Conduct Medal and Military Medal – also developed Trench Foot in November 1916 and German Measles while in camp in England waiting for his eventual return to Australia. Sgt Strachan was also wounded in action on the Somme in 1918 before eventually returning home to Australia in 1919.
Influenza and pneumonia were the cause of death for the five men of the 22nd Battalion that died in France or Belgium from non-combat related causes as shown in Figure 5a above. For the 5th/22nd influenza was the second most prevalent disease with a total of 21 cases during the war, second only to venereal disease as the most common form of hospitalisation for this group (Figure 9). In the camps and hospitals attempts were made to reduce the chance of catching a respiratory disease by better ventilation and positioning of beds.
United Kingdom – AIF depots and training camps
 In October 1914 the first Anzac contingent sailed from Australia and New Zealand for England before being diverted to Egypt on account of the concerns that the camps and facilities on the Salisbury Plain were not adequate to meet the needs of the arriving divisions in winter. The camps of Wiltshire were already having to cope the British ‘New Army’ plus the incoming Canadians, during what turned out to be a very wet winter leading to sickness and dozens of deaths amongst the new arrivals. By the summer of 1916 the camps of Wiltshire and Dorset were ready for the arriving reinforcements from Australia along with the recuperating sick and wounded of the AIF from the fighting in France. Some of these camps, notably Larkhill, Rollestone and Perham Down were exposed and bleak, but a lack of learning from the experience of the Canadians in 1914-15 meant the camps were not adequately prepared for winter on the Plain. The 1916-17 winter saw an increase in disease in the AIF depots in the UK, when during the first quarter of 1917, 123 deaths out of a total of 158 that occurred in the depot camps were from pneumonia and broncho-pneumonia, many having just disembarked the transports from Australia, including Pte Bollom, Pte Collett, Pte Gratton, Pte Moloney and Pte Canham of the 22nd Battalion. Coupled with the increase in admissions from France and the Somme as a result of Trench Foot meant that the winter of 1916-17 was by far the worse in terms of non-combat wastage for the AIF on the Western Front as shown above in ‘Graph 9’, and Figure 8 for the case study 5th/22nd Battalion.
In October 1914 the first Anzac contingent sailed from Australia and New Zealand for England before being diverted to Egypt on account of the concerns that the camps and facilities on the Salisbury Plain were not adequate to meet the needs of the arriving divisions in winter. The camps of Wiltshire were already having to cope the British ‘New Army’ plus the incoming Canadians, during what turned out to be a very wet winter leading to sickness and dozens of deaths amongst the new arrivals. By the summer of 1916 the camps of Wiltshire and Dorset were ready for the arriving reinforcements from Australia along with the recuperating sick and wounded of the AIF from the fighting in France. Some of these camps, notably Larkhill, Rollestone and Perham Down were exposed and bleak, but a lack of learning from the experience of the Canadians in 1914-15 meant the camps were not adequately prepared for winter on the Plain. The 1916-17 winter saw an increase in disease in the AIF depots in the UK, when during the first quarter of 1917, 123 deaths out of a total of 158 that occurred in the depot camps were from pneumonia and broncho-pneumonia, many having just disembarked the transports from Australia, including Pte Bollom, Pte Collett, Pte Gratton, Pte Moloney and Pte Canham of the 22nd Battalion. Coupled with the increase in admissions from France and the Somme as a result of Trench Foot meant that the winter of 1916-17 was by far the worse in terms of non-combat wastage for the AIF on the Western Front as shown above in ‘Graph 9’, and Figure 8 for the case study 5th/22nd Battalion.
As well as the local outbreaks, each arriving troopship – as discussed previously and also the case in Egypt – brought new cases of contagious diseases such as mumps and measles from Australia. The problem for AIF Depots was that these new cases were infecting the drafts being prepared for France, therefore a scheme of separation and isolation in the camps was put in place from the end of March 1917, and as a result the number of cases greatly reduced. Improvement were also made to the accommodation including ventilation for the next winter of 1917-18, and for the twelve months from July 1917 to end of June 1918 deaths numbered 141 (three per thousand per annum) as compared with nearly 300 for the first half of 1917. However these improvements were unable to stop the last of the medical crises impacting the soldiers at the end of the war. During the period between the German Spring Offensive of March 1918 and the great Allied Offensive of 8th August, medical cases, of which influenza was now a significant factor, was greater than surgical. By October 1918 the Australian General Hospitals reported the outbreak of influenza which turned into the influenza pandemic of 1918-19 that affected millions of people throughout the world.
 Tragically many men that had served with the AIF from the Anzac Landings and were given leave to England in October 1918 contracted the pneumonic phase of the influenza epidemic, resulting in deaths. Seven men from the 22nd Battalion died from either influenza or broncho-pneumonia between November 1918 and May 1919 in the camps of Europe, at sea, or for Lieut. Wymond upon arrival back in Australia. The last soldier of the 22nd Battalion to lose his life while still serving in the AIF was 2nd Cpl Knell, one of the veterans of Anzac, who died from cancer in January 1920 and is buried in the St. Mary’s Churchyard, Harefield (photograph above) alongside 111 of his comrades from the AIF that died at the nearby 1st Australian Auxiliary Hospital from sickness or wounds.
Tragically many men that had served with the AIF from the Anzac Landings and were given leave to England in October 1918 contracted the pneumonic phase of the influenza epidemic, resulting in deaths. Seven men from the 22nd Battalion died from either influenza or broncho-pneumonia between November 1918 and May 1919 in the camps of Europe, at sea, or for Lieut. Wymond upon arrival back in Australia. The last soldier of the 22nd Battalion to lose his life while still serving in the AIF was 2nd Cpl Knell, one of the veterans of Anzac, who died from cancer in January 1920 and is buried in the St. Mary’s Churchyard, Harefield (photograph above) alongside 111 of his comrades from the AIF that died at the nearby 1st Australian Auxiliary Hospital from sickness or wounds.
Casualty impact on fighting strength
Learning from the experiences of Gallipoli when infected men were frequently left far too long at the front where their condition would deteriorate plus act as a source to infect other men, troops on the Western Front were screened more rigorously and readily withdrawn if infected. However the time that each casualty was away from the unit was potentially lengthy. With the exception of minor complaints which could be dealt with at the Field Ambulance, the majority of cases were admitted to one of the General or Stationary Hospitals many miles from the front or shipped to one of the hundreds of hospitals back in the UK, a return-to-unit process which could typically last between one to three months including transit through the Command Depots. However investigation of the detailed service records of the men of the AIF illustrates a situation of significant amount of time away from unit.
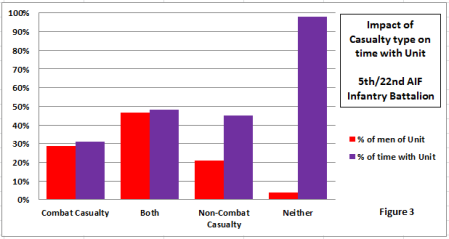 Using the 154 men of the 5th/22nd as a case study covering the period from the training camps of Egypt to the Western Front, removing the 116 men that had been a combat casualty at some point in the war (killed, wounded or both), together with the six men who went through the entire war without requiring some form of hospital treatment, this left 32 men or 20% of the group that were hospitalised with sickness or disease. Between them the remaining 32 non-combat casualties accounted for 67 non-combat cases of hospital admission – approximately two cases per man – but as can be seen in Figure 3 they were available to their unit for only 45% of the time on average. This surprisingly low figure compares with 31% for the combat casualties only, many of whom were either killed or severely wounded within the first seven months during the fighting at Pozieres. Translating this in to time, with the 5th/22nd being on active service for 137 weeks from the time they were Taken on Strength on 8th January 1916 to Armistice Day, this means that on average the non-combat casualties amongst this case study group were spending 62 weeks with their unit but 75 weeks in the hospitals, camps, some in detention as a result of disciplinary action on account of going Absent without Leave during which they caught a venereal disease, or – as was the case for fifteen, i.e. half of these men – having been discharged early as a result of their medical condition. Therefore it can be seen that non-combat wastage was having as much a detrimental impact as losses due to combat on the fighting strength of the AIF infantry battalions during the war.
Using the 154 men of the 5th/22nd as a case study covering the period from the training camps of Egypt to the Western Front, removing the 116 men that had been a combat casualty at some point in the war (killed, wounded or both), together with the six men who went through the entire war without requiring some form of hospital treatment, this left 32 men or 20% of the group that were hospitalised with sickness or disease. Between them the remaining 32 non-combat casualties accounted for 67 non-combat cases of hospital admission – approximately two cases per man – but as can be seen in Figure 3 they were available to their unit for only 45% of the time on average. This surprisingly low figure compares with 31% for the combat casualties only, many of whom were either killed or severely wounded within the first seven months during the fighting at Pozieres. Translating this in to time, with the 5th/22nd being on active service for 137 weeks from the time they were Taken on Strength on 8th January 1916 to Armistice Day, this means that on average the non-combat casualties amongst this case study group were spending 62 weeks with their unit but 75 weeks in the hospitals, camps, some in detention as a result of disciplinary action on account of going Absent without Leave during which they caught a venereal disease, or – as was the case for fifteen, i.e. half of these men – having been discharged early as a result of their medical condition. Therefore it can be seen that non-combat wastage was having as much a detrimental impact as losses due to combat on the fighting strength of the AIF infantry battalions during the war.
Conclusion
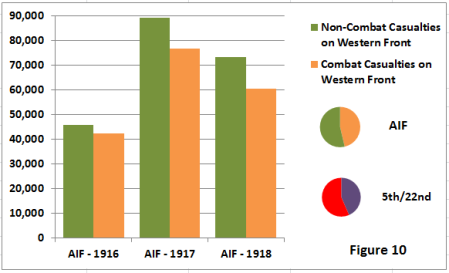 Gallipoli and Egypt could be seen as the transition point from a time when just a decade before more troops would die from serious non-combat related diseases than in battle, to a point at the end of the war in 1918 when the serving soldiers would be exposed to the same non-combat mortality risks as the wider civilian population. However despite great improvements in the field of medicine at the beginning of the last century and the deeper understanding of the causes of disease that led to the decrease in non-combat casualty deaths, sickness and disease – as shown in hospitalisation rates in Figure 2 above plus total casualty numbers in Figure 10 – still provided the most common cause of manpower wastage during the Great War. When combined with the length of time that the casualty would be away from his unit as illustrated in the previous section (Figure 3), then sickness and disease did have a significant impact on the fighting strength of the AIF during the First World War.
Gallipoli and Egypt could be seen as the transition point from a time when just a decade before more troops would die from serious non-combat related diseases than in battle, to a point at the end of the war in 1918 when the serving soldiers would be exposed to the same non-combat mortality risks as the wider civilian population. However despite great improvements in the field of medicine at the beginning of the last century and the deeper understanding of the causes of disease that led to the decrease in non-combat casualty deaths, sickness and disease – as shown in hospitalisation rates in Figure 2 above plus total casualty numbers in Figure 10 – still provided the most common cause of manpower wastage during the Great War. When combined with the length of time that the casualty would be away from his unit as illustrated in the previous section (Figure 3), then sickness and disease did have a significant impact on the fighting strength of the AIF during the First World War.
With the exception of respiratory tract diseases that caused a fifth of hospital admissions on the Western Front and included some of the potentially most serious illnesses such as influenza, pneumonia and broncho-pneumonia, many of the most common causes of manpower wastage were from types of sickness that could be addressed or avoided. Trench Foot was a serious problem in the winter of 1916-17 on the Somme, but data and literature support the notion that the affliction could be reduced through education and actions, as demonstrated in the Ypres sector of the following winter (zero cases for the 5th/22nd). Similarly outbreaks of scabies caused by the mite and PUO from lice were reduced through effective laundry facilities and better sanitation. However one of the main causes of evacuation from a unit and hence a big impact on fighting strength and completely avoidable was venereal disease, but this remained an issue particularly for the AIF for the duration of the war.
 The impact of non-combat casualties on wastage and therefore on fighting strength had been significant in conflicts past and remained so for the AIF for the duration of the First World War. Although the conditions at Gallipoli were challenging, nevertheless opportunities were missed early on to limit the debilitating impact that disease had on the men in this campaign. On the Western Front the environment and general conditions were far better, thus the ability to manage non-combat manpower wastage became more of an organisational, education and implementation issue. However the numbers of sick that had to be treated were vast and set against the backdrop of combat carnage being delivered on an industrial scale the low mortality rate from non-combat related causes is testament to the skill and dedication of the medical services.
The impact of non-combat casualties on wastage and therefore on fighting strength had been significant in conflicts past and remained so for the AIF for the duration of the First World War. Although the conditions at Gallipoli were challenging, nevertheless opportunities were missed early on to limit the debilitating impact that disease had on the men in this campaign. On the Western Front the environment and general conditions were far better, thus the ability to manage non-combat manpower wastage became more of an organisational, education and implementation issue. However the numbers of sick that had to be treated were vast and set against the backdrop of combat carnage being delivered on an industrial scale the low mortality rate from non-combat related causes is testament to the skill and dedication of the medical services.
Sources:
Official History of the Australian Army Medical Services, 1914–1918: Volume I Gallipoli, Palestine and New Guinea; Volume II – The Western Front
National Archives of Australia, Series B2455 – service records of the 5th/22nd, 6th Inf Bgde, AIF

 FIRST WORLD WAR TIMELINE
FIRST WORLD WAR TIMELINE